The pausing of elective care at the start of the Covid-19 pandemic in late March 2020 resulted in the greatest backlog in NHS history, with 6.1 million still on NHS waiting lists by March 2022, including 24,000 waiting more than two years. The Omicron variant and frequent staff shortages throughout the winter months did little to assist the situation, with the National Audit Office (NAO) predicting that waiting lists will continue to grow to between 7 and 12 million by March 2025.
As healthcare providers and Health Boards across the country battle to tackle their elective care backlogs, it has become clear that one specialty in particular has been greatly affected.
Women’s health took a backseat throughout the pause of elective care and with the redeployment of staff to more critical specialisms, the already extensive waiting lists were further added to. Throughout the pandemic, the key focus for Obstetrics and Gynaecology (O&G) departments was to deliver safe and urgent maternity services, prioritising the diagnosis and treatment of gynaecological cancers and delivering acute services relating to problems that occur in early pregnancy. Indeed, a study undertaken by the Royal College of Obstetricians and Gynaecologists (RCOG) demonstrated that around 53% of healthcare providers redeployed consultants and Speciality Associate Specialists (SAS) to support obstetrics, with 50% of gynaecologists moving to emergency obstetrics. This meant that essential elements, such as acute surgical procedures, post pregnancy care and female cancer services became under prioritised.
Since the start of the Covid-19 pandemic, gynaecology waiting lists have continued to rise dramatically, with a combined total of 570,000 women on waiting lists across the UK by December 2021. Waits soared by 60%, sharper than any other speciality, with more than 1,300 in England alone left on waiting lists for over two years, however the LCP suggests that this does not reflect the true magnitude of the problem at hand. Alongside the debilitating effects that such issues can have on daily life, conditions such as endometriosis and fibroids can lead to fertility issues should they be left untreated and with many waiting for surgery prior to beginning treatment and an age limit for IVF on the NHS, many women have been left in devastating situations. In a survey conducted by the RCOG of 837 women, 80% of women stated that they had suffered from impacts to their mental health, with 61% admitting to feeling despair at the long waits and a further 63% feeling ignored.
The pandemic has highlighted the true extent of regional health inequalities across the UK, with a report by the Health Foundation in July 2021 demonstrating that those in less affluent and minority communities more likely to suffer more severe consequences of both Covid-19 and the implications that subsequently follow. Indeed, for gynaecology 8 out of the 10 worst affected Clinical Commissioning Groups (CCGs) were located in the North West of the UK, exacerbating the need to address geographical variations in care. Extending on this, following a call for evidence by the Department of Health and Social Care in March 2021 it was revealed that just 2 in 5 women feel that they can conveniently access healthcare services locally. The key findings that would improve services included better geographical diversity, improved education of GPs and an increase in specialists in women’s health conditions. In order to successfully tackle the growing gynaecological elective backlog it is clear that a localised approach is needed to address the areas in which regional disparities are greatest, bringing the ‘postcode lottery’ for gynaecological care to an end.
In late 2021 the Royal College of Surgeons (RCS) published a report calling for the introduction of elective surgical hubs to tackle the elective care backlogs faced by healthcare providers and Health Boards across the UK. The introduction of standalone surgical facilities not only provides additional clinical capacity quickly and efficiently, but they also maximise infection control within healthcare settings, increasing both patient and staff confidence and therefore reducing the number of patients that do not turn up for planned care appointments. The flexible nature of these Healthcare Spaces ensures that facilities can be tailored to bespoke local requirements, ensuring that waiting lists in acute gynaecological care can be addressed accordingly, freeing up space within the main hospital for more complex procedures, such as emergency obstetrics.
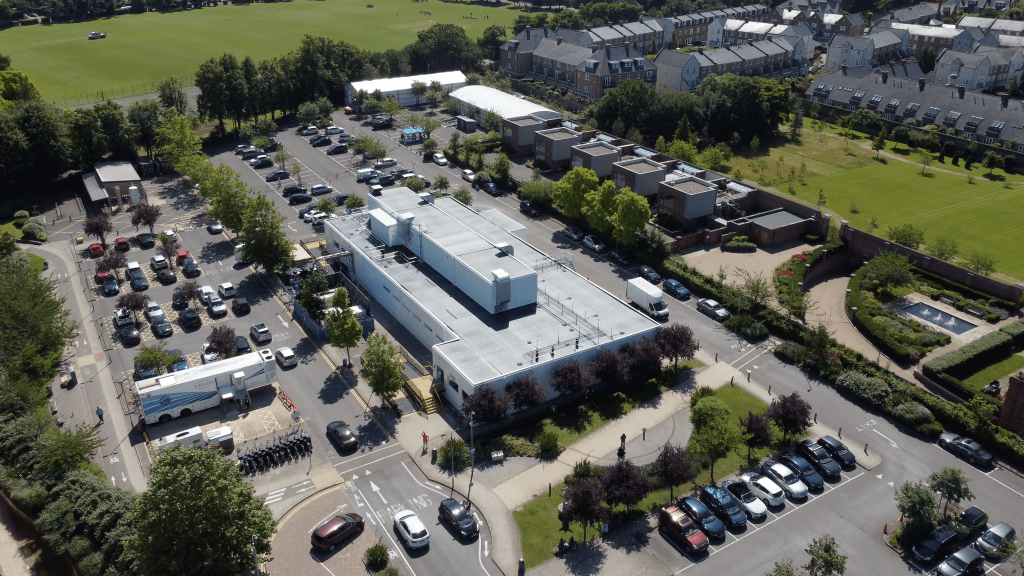
The introduction of flexible Healthcare Spaces has been successful in supporting increases in demand for maternity services in the Netherlands through the introduction of a mobile delivery suite at the Wilhelmina Hospital in Assen. The fully equipped delivery room was seamlessly linked to the main hospital and 125 babies were born in the facility throughout the duration of the contract. The introduction of this bespoke maternity facility demonstrates the effectiveness of expanding women’s health facilities in order support the growing strains on maternity services and supports the wider calls for the implementation of surgical hubs and additional capacity solutions to reduce acute care waiting lists.
Furthermore, it has been estimated that nearly 1.5 million women had breast cancer screenings delayed by between 2 and 7 months between July 2020 and June 2021, leading to around 687 additional deaths from breast cancer, screen-detected tumour deaths and DCIS. Breast screening services were suspended in late March 2020, with facilities only available for those with higher risk or those with existing findings and this was only resumed by invitation the following September. As a result of heightened infection control measures, staff shortages and strains on capacity, screening services did not resume to previous capacity levels, creating further risk for undiagnosed patients. This has led to increased calls for funding for community diagnostic centres (CDCs), particularly in areas where access to healthcare is less readily available.
Breast screening reduces the number of deaths from breast cancer by 1,300 per year, highlighting the importance of implementing community services to encourage early detection. This month it was announced that CDCs had delivered more than 700,000 additional tests across the 73 centres already in place in England, bringing healthcare services to local communities and assisting in reducing regional health inequalities.
There is still much to be done in tackling the gender disparity in care across the UK, with the RCOG calling for an overhaul of the prioritisation of care to recognise the hidden suffering experienced with women’s health conditions. Elective recovery plans should address alarming growth of gynaecological waiting lists in comparison to other specialisms, including support for local solutions and the use of surgical hubs. Flexible solutions to increase both surgical and screening capacity, particularly in areas where access to healthcare facilities is more scarce, will not only assist in reducing waiting lists, but they will contribute to an overall better quality of life for women suffering.



Q-bital Healthcare Solutions
Unit 1144 Regent Court, The Square, Gloucester Business Park, Gloucester, GL3 4AD
